Key takeaways:
- AI in healthcare is transforming clinical decision-making from diagnosis to treatment.
- AI-powered tools enhance accuracy, efficiency, and patient outcomes while reducing clinician burden.
- Successful AI implementation requires clean data, ethical considerations, and seamless integration.
- Entrepreneurs have a significant opportunity to leverage AI services for healthcare innovation.
Imagine a world where a doctor, faced with a complex patient case, doesn’t just rely on years of experience and a handful of recent studies, but has an intelligent co-pilot. This co-pilot instantly sifts through millions of patient records, the latest research papers, and diagnostic images, offering insights and probabilities that would take a human clinician weeks, if not months, to uncover. This isn’t science fiction; this is the reality being shaped by AI in clinical decision making.
Consider the recent breakthrough announced in March 2025, where researchers at the University of Cambridge unveiled an AI tool capable of expediting celiac disease diagnoses. This algorithm, trained on over 4,000 images, matches the diagnostic accuracy of pathologists while delivering results significantly faster, thereby drastically reducing patient waiting times.
This real-world example vividly illustrates how AI is empowering clinicians to make smarter decisions, moving beyond theoretical concepts to tangible improvements in patient care. The demand for sophisticated AI in healthcare decision support systems is burgeoning, presenting an unparalleled chance for businesses to innovate and lead.
For entrepreneurs and healthcare decision-makers, this transformation offers unprecedented opportunities to improve patient outcomes while building profitable, scalable businesses. The evidence is compelling: organizations implementing AI in clinical decision support report faster diagnoses, reduced errors, and significant cost savings.
Let’s get a clear and wider picture of how AI helps clinicians make faster and smarter decisions
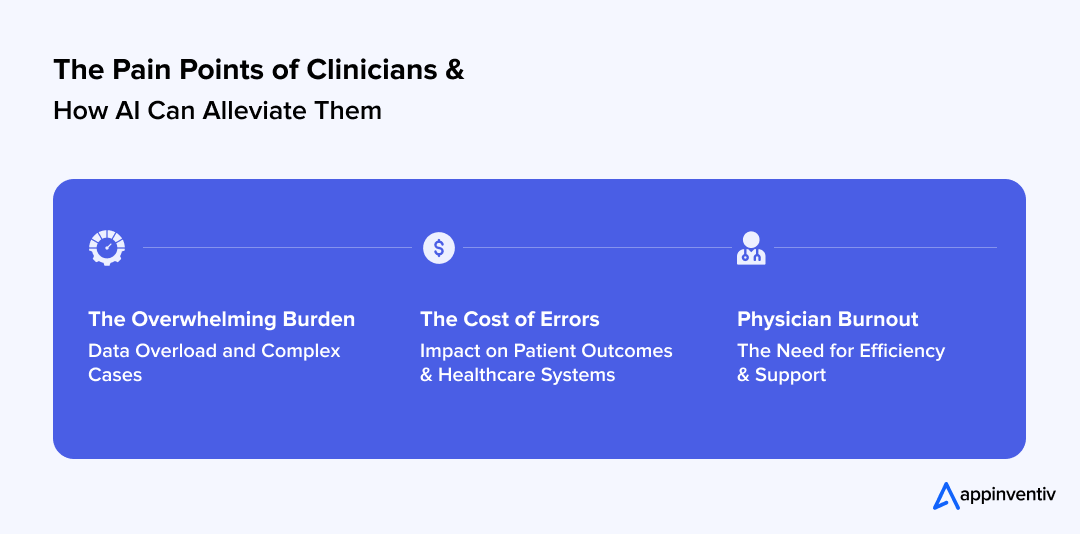
The Growing Pressure on Clinicians: Why Smarter Decisions Are Crucial
Adoption of AI in healthcare is not just a tale of innovation; it’s a matter of survival. In a world where every minute counts, AI is empowering clinicians to not only keep pace with industry demand but also overcome sudden challenges, such as the COVID-19 pandemic. At the time of such a crisis, AI has proven to be a lifesaver, enabling clinicians to make critical decisions in the most trying times. Let’s dive deeper to understand how AI helps address clinicians’ pain points:
The Overwhelming Burden: Data Overload and Complex Cases
Healthcare data is exploding. Electronic Health Records (EHRs), medical imaging, genomic sequencing, wearable device data, and real-time patient monitoring all contribute to a deluge of information that can easily overwhelm even the most experienced clinician. Diagnosing rare diseases, understanding intricate drug interactions, or predicting the trajectory of a chronic illness requires processing vast, often unstructured, datasets.
This data overload significantly increases the cognitive burden on physicians, making comprehensive AI-assisted decision-making in healthcare not just an advantage but a necessity.
The Cost of Errors: Impact on Patient Outcomes and Healthcare Systems
In healthcare, a decision made in haste or based on incomplete information can have severe consequences. Medical errors are a significant cause of morbidity and mortality, impacting patient trust and incurring immense financial costs for healthcare systems globally. The pursuit of perfection is an inherent part of medicine, and any tool that can reduce the risk of error, such as a robust AI medical decision support system, becomes invaluable.
Physician Burnout: The Need for Efficiency and Support
The unrelenting pressure of clinical practice, coupled with administrative burdens and time constraints, has led to a widespread epidemic of physician burnout.
Empowering Clinicians with AI offers a pathway to alleviate this burden by automating routine tasks, streamlining workflows, and providing rapid access to critical information, freeing up clinicians to focus on direct patient care and complex problem-solving. This shift allows for more human-centric care, which is the ultimate goal of leveraging AI in medicine.
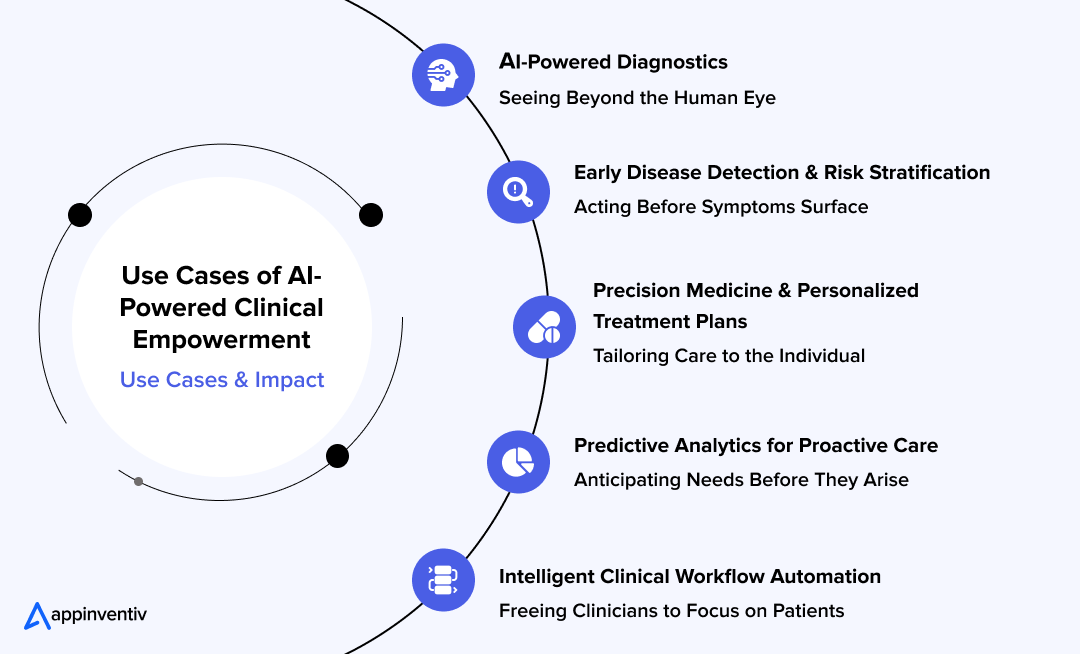
Key Pillars of AI-Driven Decision Support for Healthcare: Use Cases and Impact
The foundation of AI for healthcare providers rests on five key pillars: enhanced diagnostic accuracy, personalized treatment planning, predictive analytics for preventive care, and intelligent workflow automation. Each pillar addresses specific clinical challenges while creating measurable business value for healthcare organizations.
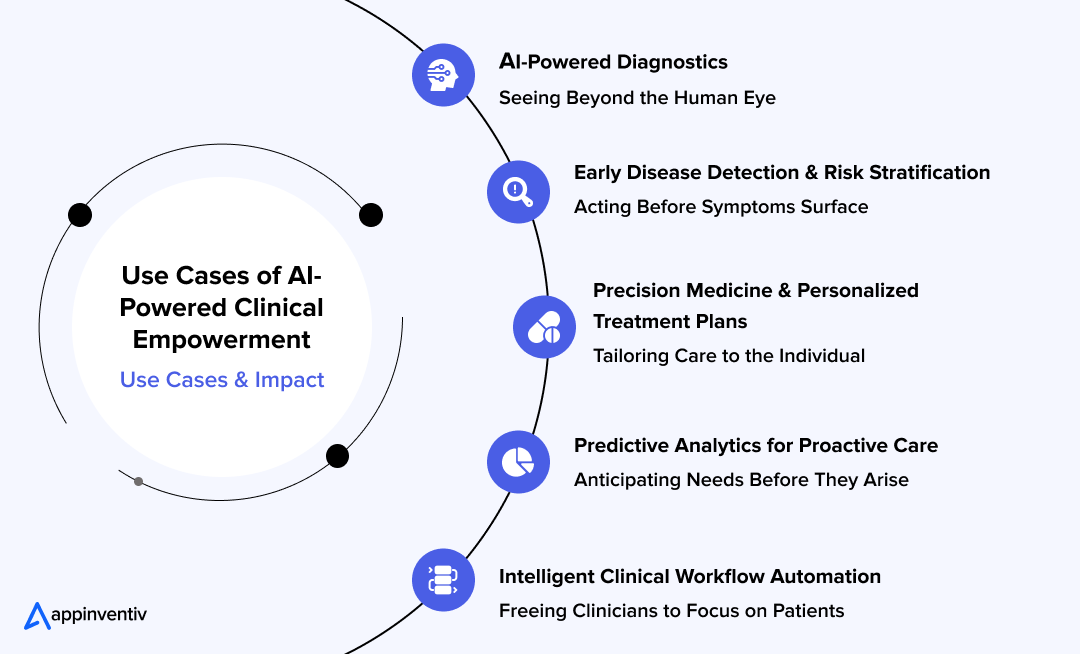
AI-Powered Diagnostics: Seeing Beyond the Human Eye
One of the most transformative areas of AI in medical decision-making lies in medical imaging analysis and diagnostics. AI algorithms can analyze medical images with a speed and precision often surpassing human capabilities.
AI models are being trained on millions of medical images—X-rays, CT scans, MRIs, and pathology slides—to detect subtle anomalies indicative of disease. For instance, AI tools like Qure.ai and Viz.ai for clinicians’ decision-making are revolutionizing radiology.
- Qure.ai has revolutionized the process of diagnosing tuberculosis and lung cancer, cutting diagnosis times from days to mere hours, even in remote areas with limited access to radiologists.
- Viz.ai analyzes CT scans to detect large vessel occlusions, a severe type of stroke, alerting specialists within minutes and significantly shortening treatment times.
- Another notable example is DiabeticU, an AI-driven diabetes management app developed by Appinventiv. DiabeticU leverages AI and ML to track blood sugar levels, identify patterns, and suggest personalized treatment plans tailored to individual needs. This allows healthcare providers to offer proactive and more accurate care to diabetic patients, drastically reducing the risk of complications and improving overall outcomes.
Early Disease Detection and Risk Stratification: Acting Before Symptoms Surface
AI and predictive decision-making in healthcare can analyze patient data—including genetic information, lifestyle factors, and medical history—to identify individuals at high risk for developing specific conditions even before symptoms appear. This proactive approach enables earlier interventions, leading to better patient outcomes and potentially preventing the progression of serious diseases.
For example, AI systems integrated with wearable devices can monitor vital signs to detect early symptoms of conditions like sepsis or atrial fibrillation, enabling timely medical intervention.
Precision Medicine & Personalized Treatment Plans: Tailoring Care to the Individual
AI also plays a significant role in precision medicine, where treatment is customized based on a patient’s unique genetic makeup. By analyzing genomic data, AI can recommend personalized treatment plans that are more likely to succeed. It also optimizes drug dosages, predicting how a patient will respond to certain treatments, thus reducing adverse reactions.
Also Read: The Role of AI in Drug Discovery and Healthcare
Predictive Analytics for Proactive Care: Anticipating Needs Before They Arise
AI-driven predictive decision support for healthcare is another breakthrough. By analyzing historical data, AI can predict which patients are at high risk for certain conditions and recommend preventive measures. This proactive approach can reduce hospital readmissions by up to 20-25% (McKinsey & Company).
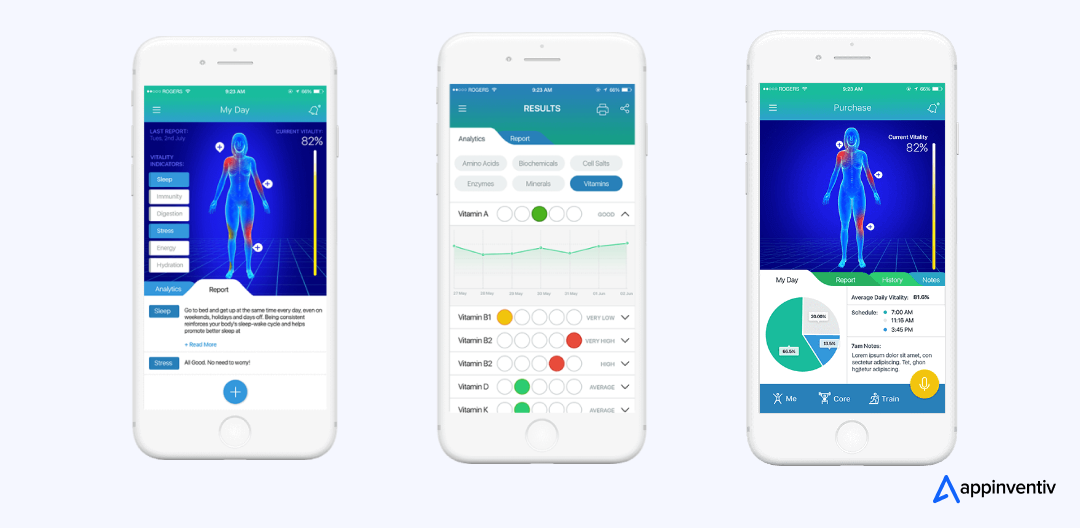
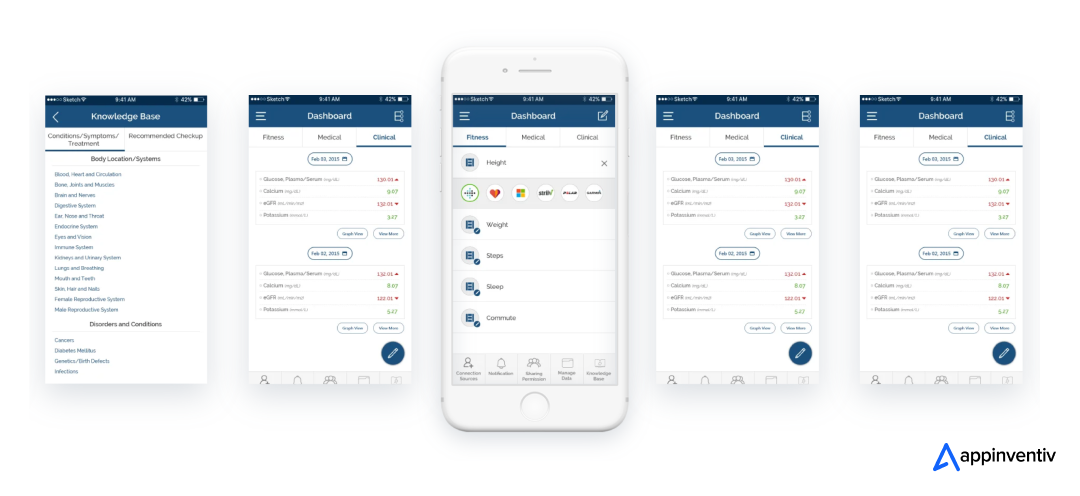
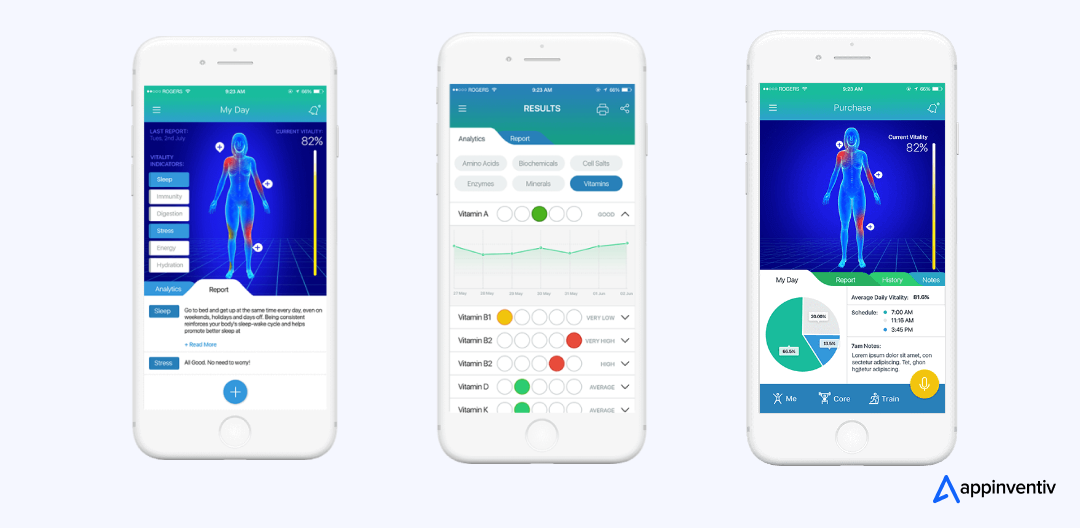
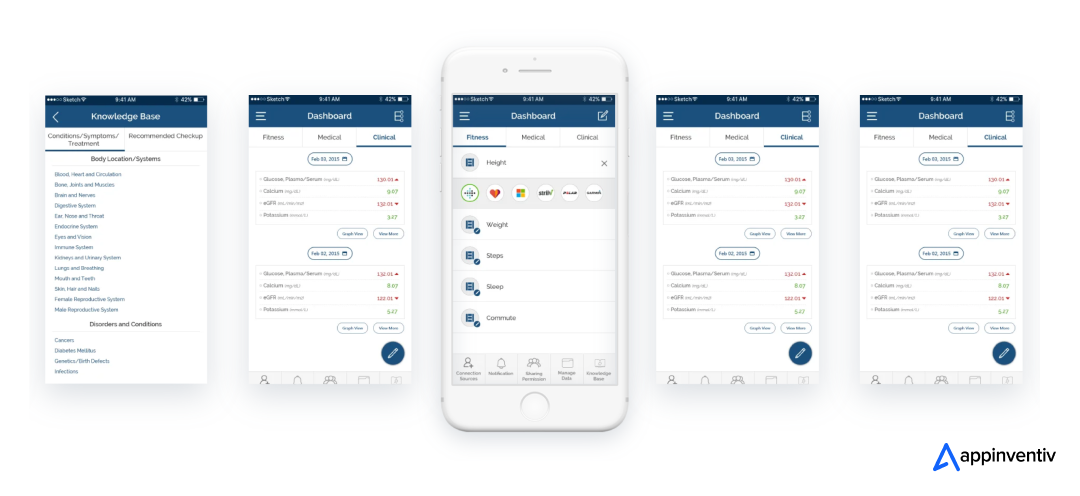
Predictive analytics is one of the key areas where AI shows immense promise. Health-e-People, a health assessment app developed by Appinventiv, is a perfect example of this. The app uses AI for healthcare decision-making, analyzing an individual’s health data to predict potential health risks and suggest preventive measures. By identifying high-risk individuals and advising on early interventions, Health-e-People improves patient outcomes and helps to prevent avoidable medical conditions, ultimately reducing healthcare costs.
Intelligent Clinical Workflow Automation: Freeing Clinicians to Focus on Patients
Beyond complex diagnostics, AI tools for clinicians’ decision-making are also revolutionizing the mundane, yet time-consuming, administrative tasks that plague clinicians. This frees up valuable time for direct patient interaction, a key aspect of Empowering Clinicians with AI.
AI for medical decision support can also significantly enhance efficiency by automating routine tasks. Generative AI can automate medical documentation, scheduling, billing, and insurance verification, reducing administrative burdens. This gives clinicians more time to focus on what truly matters—patient care. Forbes expects that AI in clinical workflow automation can save around $18 billion for the healthcare industry, as machines can help healthcare providers save time on repetitive tasks.
Benefits of AI in Clinical Decision Making: Why Smart Decision-Making with AI is No Longer Optional
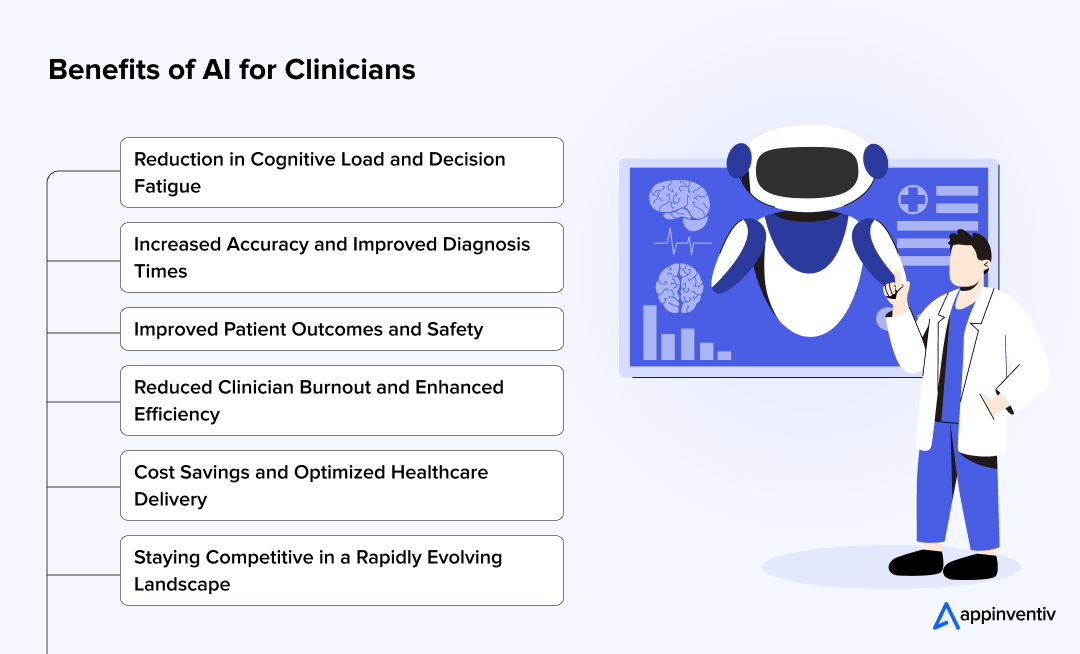
The benefits of AI in healthcare decision-making extend far beyond mere technological advancement; they represent a fundamental shift towards a more efficient, accurate, and humane healthcare system. Here are some of the most common benefits of AI-driven decision-making in healthcare:
Reduction in Cognitive Load and Decision Fatigue
By offloading data analysis and routine tasks, AI-driven decision-making tools for healthcare providers significantly reduce the mental burden on clinicians, allowing them to conserve their cognitive energy for complex, high-stakes decisions and empathetic patient interactions.
Increased Accuracy and Improved Diagnosis Times
AI’s ability to process vast amounts of data and identify subtle patterns often leads to more accurate diagnoses and significantly faster diagnostic turnaround times, especially in fields like radiology and pathology.
Improved Patient Outcomes and Safety
Ultimately, the enhanced accuracy and efficiency brought by AI decision support in healthcare outcomes directly translate to better patient care, fewer medical errors, and improved safety. Early detection, personalized treatments, and proactive interventions all contribute to superior health outcomes.
For example, Appinvetiv developed Soniphi, a Vitality Health App that demonstrates how AI can contribute to proactive health management and improved patient outcomes. This innovative solution analyzes voice samples to assess an individual’s vitality and provides personalized insights into their well-being. While not a direct diagnostic tool for clinicians, the aggregated, AI-processed data from such platforms can inform healthcare providers about population health trends, potential risks, and the effectiveness of lifestyle interventions, allowing for more data-driven public health and preventive care strategies.
Reduced Clinician Burnout and Enhanced Efficiency
By automating administrative tasks and providing intelligent support, Empowering Clinicians with AI helps alleviate the root causes of burnout, leading to more engaged, satisfied, and productive healthcare professionals.
Cost Savings and Optimized Healthcare Delivery
More accurate diagnoses, reduced readmissions, optimized resource allocation, and streamlined workflows contribute to significant cost savings across the healthcare continuum, making healthcare more sustainable.
Staying Competitive in a Rapidly Evolving Landscape
For healthcare organizations and entrepreneurs looking to make their mark, adopting and leveraging AI-powered decision support in medicine is no longer a luxury but a strategic imperative to remain competitive and deliver cutting-edge care.
Also Read: The uses and benefits of artificial intelligence in clinical trials
Best Practices to Get Started with AI-Powered Decision Support Tools
Implementing AI effectively in healthcare is not simply about developing an AI application; it requires a strategic, thoughtful approach. For businesses seeking to leverage the power of custom AI development in healthcare, understanding these nuances is critical. Here are some best practices to integrate AI in healthcare service delivery
Data is King (and Clean Data is Gold)
For AI to work effectively in healthcare, data quality is crucial. Clean, accessible, and interoperable data from electronic health records (EHRs) and other systems is necessary for AI systems to generate meaningful insights. Addressing data silos and ensuring data standardization across platforms is the first step toward successful AI integration.
Overcoming the “Black Box” Challenge: Explainable AI
Trust in AI-driven recommendations requires transparency in algorithmic decision-making. Explainable AI initiatives ensure that clinicians understand how AI systems reach their conclusions, enabling informed clinical judgment while maintaining accountability for patient care decisions.
Healthcare organizations must prioritize AI solutions that provide clear reasoning pathways and allow clinician override capabilities. This approach preserves clinical autonomy while providing the benefits of AI-enhanced decision-making.
Addressing Bias and Ethical Considerations
While AI systems offer significant benefits, it’s crucial to ensure that algorithmic bias doesn’t skew decision-making. For instance, if AI is trained on biased data, it may disproportionately misdiagnose certain groups of people. Mitigating these biases through careful training and diverse datasets is key to the ethical deployment of AI in healthcare.
Seamless Integration with Existing Systems
Successful AI implementation requires minimal disruption to existing clinical workflows. Thus, organizations should develop advanced AI platforms that can scale easily and integrate smoothly with current EHR systems, PACS networks, and clinical protocols. Phased implementation approaches allow gradual adoption while monitoring performance and user acceptance.
Overcoming Challenges in AI-Assisted Decision-Making & Solution
While AI-assisted decision-making in healthcare holds immense potential, the path to seamless implementation is not without its challenges. The integration of AI into clinical workflows requires careful consideration and a structured approach to overcome several hurdles. Here, we explore several strategies to overcome AI challenges in healthcare to ensure the successful adoption of AI in healthcare.
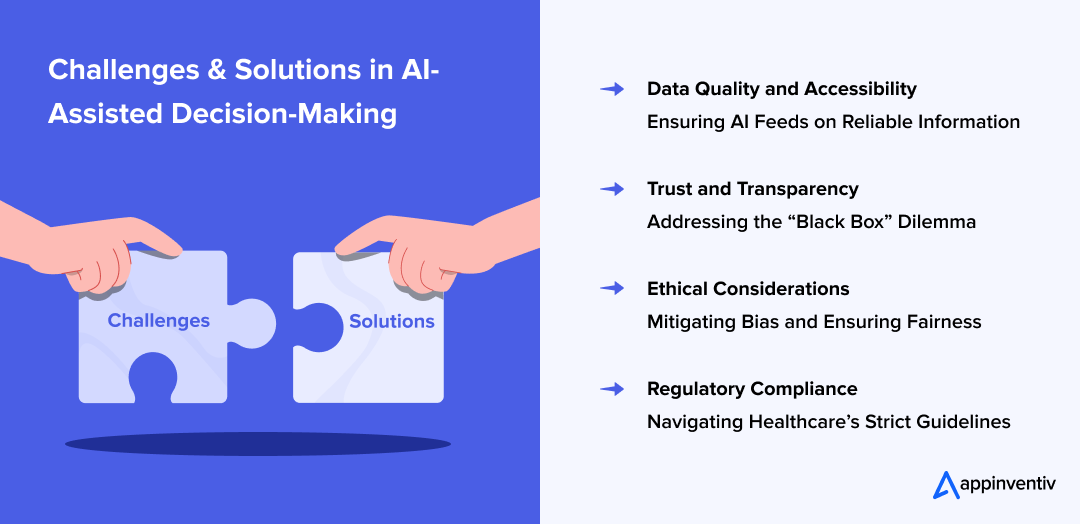
1. Data Quality and Accessibility: Ensuring AI Feeds on Reliable Information
Challenge: One of the biggest obstacles to the successful implementation of AI-powered clinical decision support systems is the quality and accessibility of data. AI systems require vast amounts of accurate, diverse, and timely data to function effectively. However, healthcare data often resides in disparate systems, leading to data silos and inconsistencies that can hinder AI performance.
Solution: To overcome this challenge, healthcare providers must prioritize data integration and ensure interoperability with healthcare systems like EHRs, PACS, and lab results.
2. Trust and Transparency: Addressing the “Black Box” Dilemma
AI algorithms, especially deep learning models, are often perceived as “black boxes” because their decision-making processes are not always transparent to end-users. Clinicians may hesitate to trust recommendations made by AI if they don’t understand how the system arrived at a particular conclusion. This lack of transparency can undermine the adoption of AI in clinical decision-making.
Solution: Explainable AI (XAI) is the key to solving this issue. By designing AI models that offer clear, interpretable insights, clinicians can better understand the reasoning behind AI-driven decisions.
3. Ethical Considerations: Mitigating Bias and Ensuring Fairness
AI models are only as good as the data they are trained on, and if the training data contains biases, AI systems can inadvertently propagate these biases. For instance, facial recognition systems in AI have shown bias against darker skin tones, and similar biases in medical AI can lead to misdiagnosis or unequal treatment recommendations for diverse patient groups. This poses a significant ethical challenge in AI-assisted decision-making in hospitals.
Solution: Healthcare providers must commit to responsible AI principles by implementing frameworks that guarantee fairness, accountability, and transparency. Also, AI systems should be trained on diverse datasets that represent a broad range of demographics.
4. Regulatory Compliance: Navigating Healthcare’s Strict Guidelines
Healthcare is a highly regulated industry; thus, AI in clinical decision-making must adhere to strict compliance standards such as HIPAA, FDA regulations, and GDPR. Ensuring that AI systems meet these regulatory requirements is crucial to avoid legal risks and ensure patient data privacy and security.
Solution: To overcome this challenge, healthcare organizations should partner with AI solution providers that are well-versed in industry regulations and can help implement AI systems that comply with healthcare compliance.
The Future of AI in Clinical Decision-Making
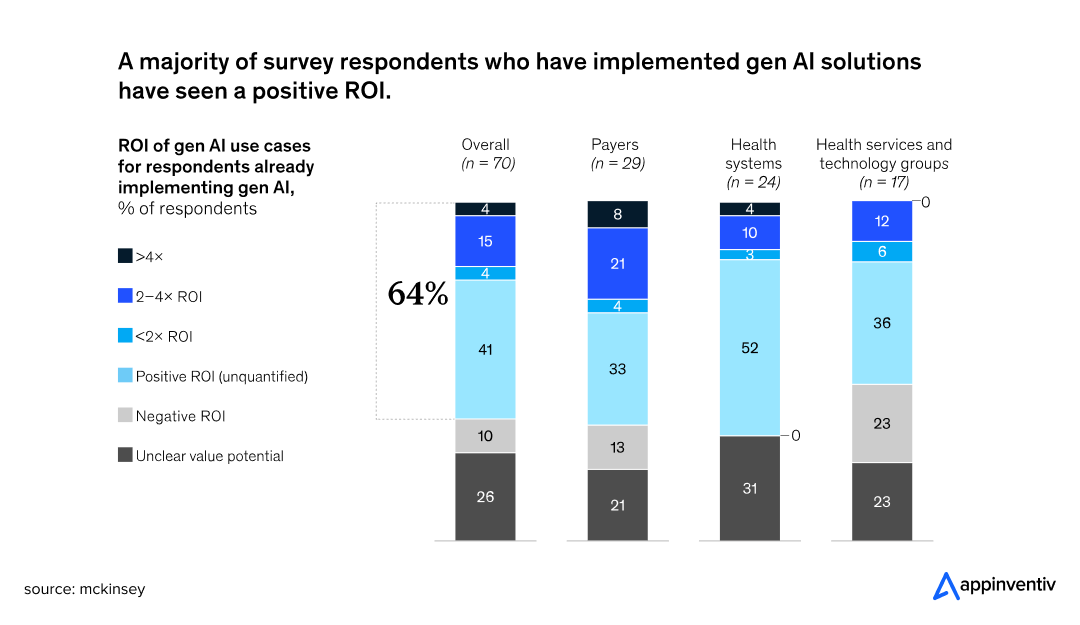
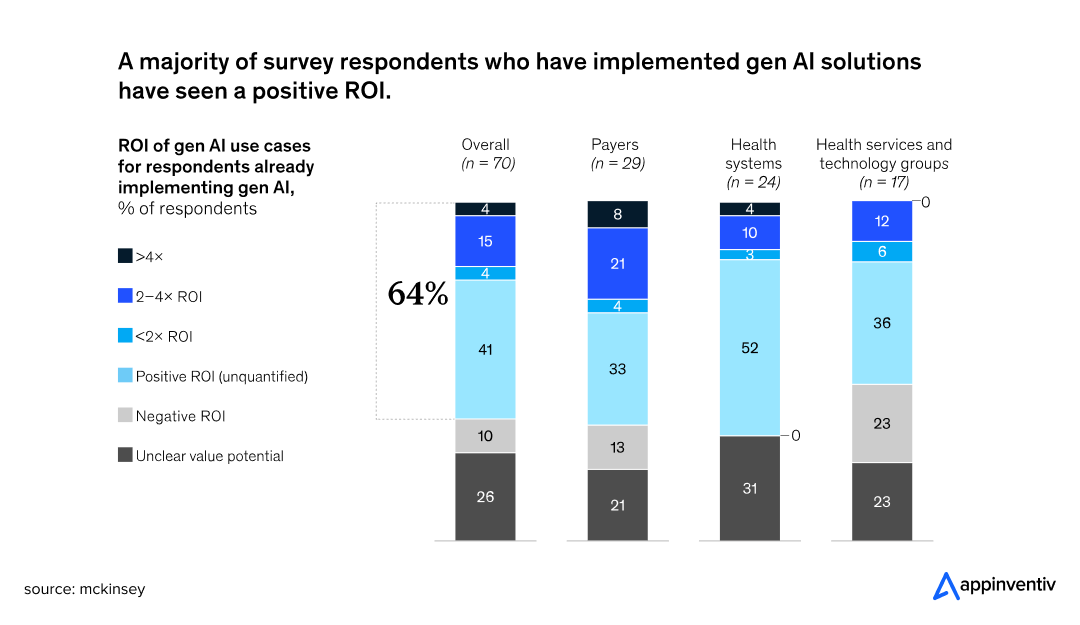
The journey of AI empowering clinicians is still in its early stages, yet the trajectory is clear: a future where AI is deeply embedded in every aspect of clinical care. This strong momentum is also reflected in organizations actively seeking to quantify the impact of their investments in advanced AI capabilities.
In fact, among those who have already implemented generative AI use cases, a significant 64% anticipate or have already quantified a positive return on investment (ROI), highlighting the high expectations and tangible benefits seen from this technology.
Some of the emerging AI trends that will redefine the healthcare landscape in the coming years are:
Generative AI
Beyond automated documentation, generative AI in healthcare could soon assist in formulating diagnostic hypotheses, summarizing complex research findings, or even drafting personalized patient education materials.
AI in Remote Patient Monitoring
As wearable technology becomes more sophisticated, AI will play a central role in analyzing continuous streams of biometric data, providing real-time alerts for potential health issues, and enabling proactive care.
Also Read: AI in Telemedicine: Use Cases, Challenges & Future Trends
Digital Twin Technology
Imagine a “digital twin” of a patient, a virtual replica where different treatment scenarios can be simulated with AI to predict outcomes before administering actual interventions. This cutting-edge application of digital twins in healthcare holds immense promise for personalized medicine.
Federated Learning
This technique allows AI models to be trained on decentralized datasets across multiple institutions without sharing raw patient data, addressing privacy concerns while still leveraging collective intelligence.
Appinventiv’s Approach to Empowering Healthcare through AI
The relentless advancements of artificial intelligence are paving the way towards truly smart decision-making in healthcare. From revolutionizing diagnostics and enabling precision medicine to streamlining workflows and providing predictive insights, AI is empowering clinicians, not just an aspiration but a rapidly unfolding reality. This paradigm shift offers immense opportunities for innovators to contribute to a healthier, more efficient, and more equitable healthcare ecosystem.
At Appinventiv, we specialize in delivering next-gen AI development services to build robust, secure, and user-centric solutions that genuinely Empower Clinicians with AI. Our expertise in custom AI development and healthcare software development services helps you create intelligent systems that seamlessly integrate with existing infrastructure, prioritize data privacy and security, and are designed with the clinician and patient at the core.
Our team of 1600+ tech experts understands the intricacies of healthcare data, the imperative for ethical AI, and the need for scalable platforms that can meet evolving industry demands. They know what it takes to build a next-gen AI platform for healthcare that can drive real results and improve patient care.
Our successful partnerships with healthcare clients like Soniphi, YouComm, DiabeticU, and Health-e-People are a testament ot our unmatched excellence in AI service delivery for
Now, the question is no longer if AI will transform healthcare, but how quickly you will leverage its power. So, rush to grab the opportunity of AI in clinical decision making and build an AI healthcare app today.
Partner with us now.
FAQs
Q. How does AI improve clinical decision-making?
A. AI improves clinical decision-making by providing clinicians with faster, more accurate insights derived from vast datasets, enabling earlier disease detection, personalized treatment plans, and optimized resource allocation, ultimately leading to better patient outcomes and reduced medical errors. It acts as an intelligent co-pilot, augmenting human expertise.
Q. What is AI in clinical decision making?
A. At its core, AI-enhanced clinical decision making involves sophisticated algorithms and machine learning models that analyze vast datasets to identify patterns, make predictions, and offer insights. This isn’t merely about automating simple, repetitive tasks; it’s about intelligent automation and insight generation.
For instance, an AI in healthcare decision support systems can process complex patient histories, lab results, and imaging scans to suggest potential diagnoses or treatment pathways that a human might overlook due to cognitive limitations or time pressures.
Q. Is AI the future of clinical decision-making?
A. Yes, AI is the future of clinical decision-making. While it will not replace human clinicians, AI will increasingly serve as an indispensable augmentative tool, enhancing diagnostic accuracy, predicting patient outcomes, automating routine tasks, and enabling precision medicine. The trend towards AI in clinical decision support systems is undeniable and growing exponentially.
Product Development & Engineering
IT Managed & Outsourcing
Consulting Services
Data Services
Didn't find what you're looking for? Let us know your needs, and we'll tailor a solution just for you.